Insulinoma
Insulinoma is the most common functioning tumor of the pancreas, and affected patients present a tableau of symptoms referable to hypoglycemia (symptoms of catecholamine release), mental confusion and obtundation. Many patients have symptoms for years. Some have been greatly troubled by emotional instability and fits of rage, often followed by somnolence.
Incidence: This tumors are so rare. Probably the best series of insulinomas is from the Olmsted County (Mayo Clinic). This study (cohort) was seen over a sixth decade period (’27 to ’86). The incidence there was 0.4 per 100,000 person-years (or four cases per million per year).
The diagnostic hallmark of the syndrome is the so-called Whipple triad, wich consists in symptoms of hypoglycemia (catecholamine release), low blood glucose level (40 to 50 mg/dL), and relief of symptoms after intravenous administration of glucose. The triad is not entirely diagnostic, because it may be emulated by factitious administration of hypoglycemic agents, by rare soft tissue tumors, or occasionally by reactive hypoglycemia. The clinical syndrome of hyperinsulinism may follow one of two patterns or sometimes a combination of both.
The symptom complex may be due to autonomic nervous overactivity, expressed by fatigue, weakness, fearfulness, hunger, tremor, sweating, and tachycardia, or alternatively, a central nervous system disturbance with apathy (or irritability or anxiety), confusion, excitement, loss of orientation, blurring of vision, delirium, stupor, coma, or convulsions.
Because cerebral tissue metabolize only glucose, prolonged profound hypoglycemia may cause permanent brain damage. Clinicians need to be alert to this when attempting to induce hypoglycemia by fasting.
Preoperative NPO orders must be accompanied by intravenous administration of glucose.
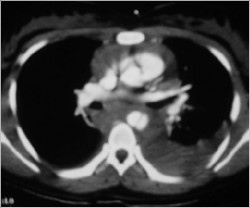
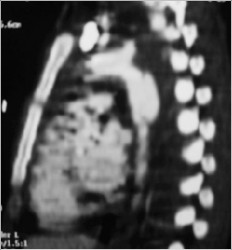
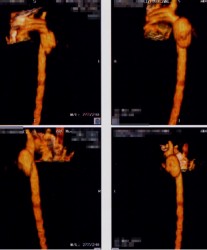
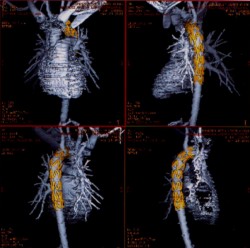
The diagnosis: Is established by demonstrating inappropriately high serum insulin concentrations during a spontaneous or induced episode of hypoglycemia. Then imaging techniques are used to localize the tumor. The available procedures include spiral CT, arteriography, ultrasonography (transabdominal and endoscopic), and 111-In-pentetreotide imaging. Transabdominal ultrasonography is our preferred initial test.
Insulinomas are small (usually smaller than 1.5 cm), usually single (only 10% are multiple and those are usually associated with MEN 1 syndrome), usually benign (only 5% to 10% are malignant), and usually hard to find. Success in localization often parallels the degree of invasiveness of the study.
Its treatment:
Treatment for insulinoma is surgical. At operation, the incision is dictated by operator preference, either a midline incision from the xiphoid to below the umbilicus or a bilateral subcostal incision. Exposure should be generous, and mechanical ring retractors are an asset. The entire abdomen should be explored, with particular attention being paid to possible liver metastases.
The head of the pancreas should be palpated carefully and examined anteriorly and posteriorly; the body and tail of the pancreas should be palpated, dividing any ligamentous attachments to the spleen, delivering the spleen into the wound, and rotating the tail anteriorly to allow palpation and visualization.
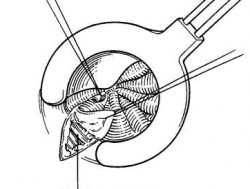
Anyone operating patients with pancreatic islet adenomas should be familiar with techniques for, and limitations of, intraoperative ultrasonography. The higher-resolution (7.5-to 10-MHz) transducers are used in the pancreas; because of its greater depth of penetration. Islet tumors are detected as sonolucent masses, usually of uniform consistency. Several reports attest to the high degree of accuracy of intraoperative ultrasound.
Review of current literature leads to the almost startling conclusion that nearly all syndromes of hyperinsulinism are due to insulinomas and that nearly all insulinomas can now be detected before or during surgery. Having said this, there appears to be scant justification for an empirical (“blindâ€) partial pancreatectomy except in patients with insulinoma plus MEN 1.
Most insulinomas are benign and can be enucleated. Nutrient vessels in the bed of the adenoma should be cauterized.
The 10% of patients with hyperinsulinism who have MEN 1 syndrome have multiple islet tumors, one of which is usually dominant and responsible for the excessive insulin output.